Health
ECTOPIC Pregnancy-Causes, Treatment & Prevention
Ectopic pregnancy (Ectopic means “out of place”) is when an embryo grows in the wrong place outside the womb. An embryo is a fertilized egg that results when an egg and sperm combine.
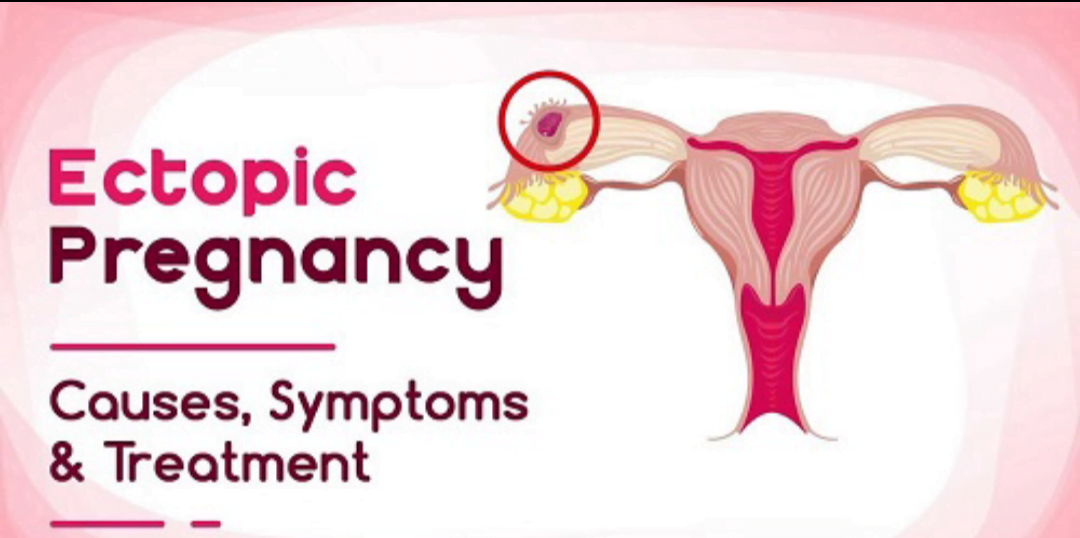
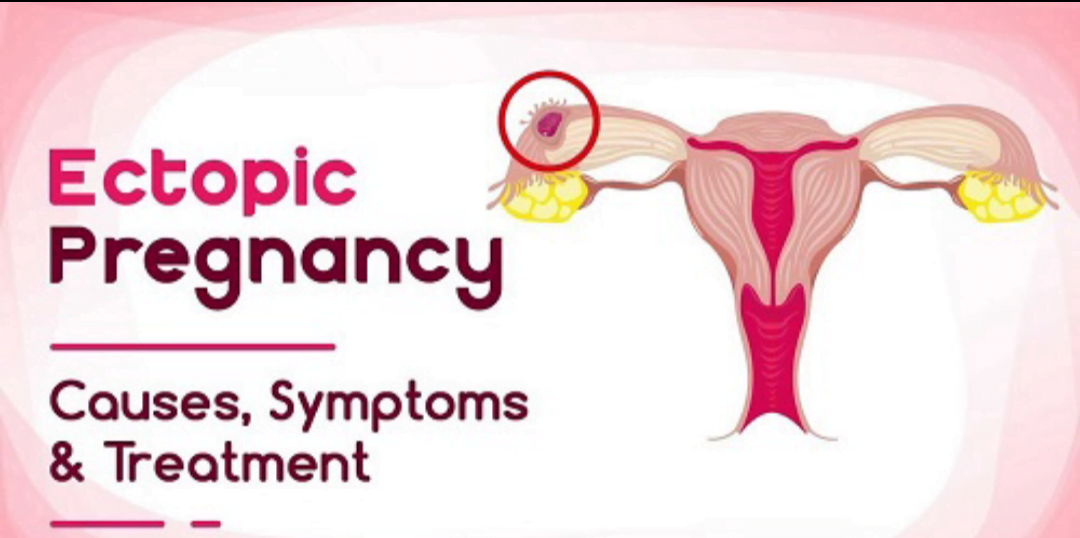
Once an egg is fertilized, it usually travels down a fallopian tube and attaches to the lining of your uterus (also called the womb). Fallopian tubes are the tubes between your ovaries (where your eggs are stored) and the uterus. The uterus is the place inside you where your baby grows.
In most ectopic pregnancies, the fertilized egg attaches to a fallopian tube before it reaches the uterus. Less often, it attaches to an ovary, the cervix or your abdomen (belly). The cervix is the opening to the uterus that sits at the top of the vagina. These areas don’t have enough space or the right tissue for a baby to grow.
Without treatment, an ectopic pregnancy can cause the place where it’s attached to bleed heavily or burst. This can lead to serious bleeding and even death in pregnant women. An ectopic pregnancy always ends in pregnancy loss. About 1 in 50 pregnancies (2 percent) in the United States is ectopic.
Types of ectopic pregnancy
Tubal pregnancy
A tubal pregnancy occurs when the egg has implanted in the fallopian tube. This is the most common type of ectopic pregnancy and the majority of ectopic pregnancies are tubal pregnancies. The type of tubal pregnancy can be further classified according to where inside the fallopian tube the pregnancy becomes established.
Non-tubal ectopic pregnancy
Nearly two percent of all ectopic pregnancies become established in other areas including the ovary, the cervix or the intra-abdominal region.
Heterotopic pregnancy
In some rare cases, one fertilized egg implants inside the uterus and another implant outside of the structure. The ectopic pregnancy is often discovered before the intrauterine pregnancy, mainly due to the painful nature of ectopic pregnancy. If human chorionic gonadotropin levels continue to rise after the ectopic pregnancy has been removed, the pregnancy inside the womb may still be viable.
Causes
An ectopic pregnancy is often caused by damage to the fallopian tubes. A fertilized egg may have trouble passing through a damaged tube, causing the egg to implant and grow in the tube.
Things that make you more likely to have fallopian tube damage and an ectopic pregnancy include:
- Smoking: The more you smoke, the higher your risk of an ectopic pregnancy.
- Pelvic inflammatory disease (PID): This is often the result of an infection such as chlamydia or gonorrhea.
- Endometriosis, which can cause scar tissue in or around the fallopian tubes.
- Being exposed to the chemical DES before you were born.
Some medical treatments can increase your risk of ectopic pregnancy. These include:
- Surgery on the fallopian tubes or in the pelvic area.
- Fertility treatments such as in vitro fertilization.
Symptoms of Ectopic Pregnancy
An ectopic pregnancy doesn’t always cause symptoms and may only be detected during a routine pregnancy scan.
If you do have symptoms, they tend to develop between the 4th and 12th week of pregnancy.
Symptoms can include a combination of:
- A missed period and other signs of pregnancy
- Tummy pain low down on 1 side
- Vaginal bleeding or a brown watery discharge
- Pain in the tip of your shoulder
- Discomfort when peeing or pooing
But these symptoms aren’t necessarily a sign of a serious problem. They can sometimes be caused by other problems, such as a stomach bug.
Risk Factors
The risk factors include the following:
- Previous ectopic pregnancy
- Prior fallopian tube surgery
- Previous pelvic or abdominal surgery
- Certain sexually transmitted infections (STIs)
- Pelvic inflammatory disease
- Endometriosis
Other factors that may increase a woman’s risk of ectopic pregnancy include
- Cigarette smoking
- Age older than 35 years
- History of infertility
- Use of assisted reproductive technology, such as in vitro fertilization (IVF)
About one-half of all women who have an ectopic pregnancy do not have known risk factors. Sexually active women should be alert to changes in their bodies, especially if they experience symptoms of an ectopic pregnancy.
Ectopic pregnancy complications
A complication of ectopic pregnancy is more likely if diagnosis or treatment is delayed, or if the condition is never diagnosed.
Internal bleeding: A woman who has an ectopic pregnancy and does not receive a timely diagnosis or treatment is more likely to experience severe internal bleeding. This can lead to shock and serious outcomes.
Damage to fallopian tubes: Delayed treatment can also result in damage to the fallopian tube, significantly increasing the risk of future ectopic pregnancies.
Depression: This can result from grieving over the loss of the pregnancy and worrying about future pregnancies.
It is important to remember that pregnancy remains possible even if a fallopian tube is removed. If both tubes are removed, in-vitro fertilization (IVF) remains an option if a woman wishes to conceive a child.
Diagnosis of ectopic pregnancy
Most ectopic pregnancies are suspected between 6 and 10 weeks of pregnancy. Sometimes the diagnosis is made quickly. However, if you are in the early stages of pregnancy, it can take longer (a week or more) to make a diagnosis of an ectopic pregnancy.
Your diagnosis will be made based on the following:
Consultation and examination
Your doctor will ask about your medical history and symptoms and will examine your abdomen. With your consent, your doctor may also do a vaginal (internal) examination. You should be offered a female chaperone (someone to accompany you) for this. You may also wish to bring someone to support you during your examination.
Urine pregnancy test
If you have not already had a positive pregnancy test, you will be asked for a urine sample so that this can be tested for pregnancy. If the pregnancy test is negative, it is very unlikely that your symptoms are due to an ectopic pregnancy.
Ultrasound scan
A transvaginal scan (where a probe is gently inserted in your vagina) is known to be more accurate in diagnosing an ectopic pregnancy than a scan through the tummy (transabdominal scan). Therefore, you will be offered a transvaginal scan to help identify the exact location of your pregnancy. However, if you are in the early stages of pregnancy, it may be difficult to locate the pregnancy on scanning and you may be offered another scan after a few days.
Blood tests
A test for the level of the pregnancy hormone βhCG (beta-human chorionic gonadotropin) or a test every few days to look for changes in the level of this hormone may help to give a diagnosis. This is usually checked every 48 hours because, with a pregnancy in the uterus, the hormone level rises by 63% every 48 hours (known as the ‘doubling time’) whereas, with ectopic pregnancies, the levels are usually lower and rise more slowly or stay the same.
Laparoscopy
If the diagnosis is still unclear, operation under a general anesthetic called a laparoscopy may be necessary. The doctor uses a small telescope to look at your pelvis by making a tiny cut, usually into the umbilicus (tummy button). This is also called keyhole surgery.
Treatment
Currently, three different treatments available for an ectopic pregnancy.
Your doctor will discuss the most appropriate one for you, however, your doctor may also find it necessary to proceed from one method to another.
Laparoscopic (keyhole) surgery to remove the fertilized egg from fallopian tubes
- A telescopic device (the laparoscope) is inserted through a small cut below your navel (belly button). To help identify your organs, carbon dioxide gas is blown into your stomach through a needle.
- A couple of small incisions are also made in your lower abdomen to manipulate and if necessary remove the ectopic pregnancy tissue.
- The surgery may involve removing your fallopian tube (salpingectomy) or opening your fallopian tube (salpingostomy) to remove the ectopic pregnancy tissue.
Laparotomy to remove the ectopic pregnancy
If the pregnancy is advanced or there has been significantly associated hemorrhaging (bleeding) then your doctor may perform a laparotomy, a type of surgery involving a much larger incision.
Intramuscular injection of the drug methotrexate
- A medication called methotrexate is used to dissolve the pregnancy tissue. It is given by injection in the leg or bottom and is suitable for women without pain or those with minimal pain.
- This type of treatment was introduced to avoid surgery but needs careful follow-up.
- The follow-up requires blood tests after the first week and then once or twice a week until tests show that you are no longer pregnant. The schedule of blood tests will be explained to you by your doctor. The treatment has a 90 percent success rate. If it is not successful, your doctor may have to reconsider medical treatment or surgery.
Recovery after treatment
- After laparoscopic surgery or a methotrexate injection, most women recover and are ready to leave the hospital within 24 hours.
- After a laparotomy, it is more common to stay in the hospital for 2 to 3 days.
- If you had a salpingostomy or methotrexate injection you will need to have regular tests at the hospital to ensure all the pregnancy cells are gone. This usually involves another blood hormone test.
Prevention of Ectopic Pregnancy
There’s no way to prevent an ectopic pregnancy, but here are some ways to decrease your risk:
- Limit your number of sexual partners.
- Always use a condom during sex to help prevent sexually transmitted infections and reduce your risk of pelvic inflammatory disease.
- Don’t smoke. If you do, quit before you try to get pregnant.














